Library
PDH complex and the TCA cycle- NBME style questions set-2
- October 25, 2024
- Posted by: Namrata Chhabra
- Category: Energy metabolism Learning resources Library Metabolism of Carbohydrates Multiple-Choice questions Multiple-choice questions Multiple-choice questions Practice questions Practice questions USMLE Content USMLE Style questions USMLE styled question bank
1. The cytosolic isoform of which of the following TCA cycle enzymes requires NADP⁺ as a coenzyme, which can be utilized in the reduced state for reductive biosynthesis?
A. Aconitase
B. Citrate Synthase
C. Isocitrate Dehydrogenase
D. Malate Dehydrogenase
E. Succinate Dehydrogenase
The correct answer is C: Isocitrate Dehydrogenase: The cytosolic isoform of isocitrate dehydrogenase (IDH) uses NADP⁺ as a coenzyme. In this reaction, isocitrate is converted to α-ketoglutarate, generating NADPH, which is essential for reductive biosynthesis processes, such as fatty acid and cholesterol synthesis. This distinguishes it from the mitochondrial isoform, which typically uses NAD⁺.
Incorrect Options:
A. Aconitase: Aconitase catalyzes the conversion of citrate to isocitrate through the intermediate cis-aconitate. It does not require NADP⁺; instead, it requires an iron-sulfur cluster for its activity.
C. Citrate Synthase: This enzyme catalyzes the formation of citrate from acetyl-CoA and oxaloacetate. It does not involve NADP⁺ or NADPH in its reaction.
D. Malate Dehydrogenase: While malate dehydrogenase catalyzes the conversion of malate to oxaloacetate, generating NADH (not NADPH), this enzyme does not use NADP⁺ as a cofactor in either the mitochondrial or cytosolic forms.
E. Succinate Dehydrogenase: This enzyme converts succinate to fumarate and is embedded in the inner mitochondrial membrane, functioning as Complex II in the electron transport chain. It uses FAD (not NADP⁺ or NAD⁺) as a cofactor.
2. Which of the following intermediates of the TCA cycle is depleted in Type 1 Diabetes Mellitus to suppress the TCA cycle and channel excess Acetyl-CoA towards the ketogenesis pathway?
A. Alpha-Ketoglutarate
B. Malate
C. Oxaloacetate
D. Pyruvate
E. Succinate
The correct answer is C. Oxaloacetate: In Type 1 Diabetes Mellitus, impaired glucose uptake reduces pyruvate production, which depletes oxaloacetate. Since oxaloacetate is necessary to combine with acetyl-CoA to form citrate in the TCA cycle, its depletion suppresses the cycle, causing excess acetyl-CoA to be diverted towards ketogenesis, resulting in the production of ketone bodies.
Incorrect Options
A. Alpha-Ketoglutarate: Though an important intermediate, its depletion does not directly channel acetyl-CoA towards ketogenesis.
B. Malate: Malate participates in gluconeogenesis, but its reduction is not the key driver of ketogenesis.
D. Pyruvate: Pyruvate is the end product of glycolysis and a precursor to acetyl-CoA, but its depletion is not the primary factor triggering ketogenesis.
E. Succinate: Succinate is involved in the TCA cycle but has no direct role in ketogenesis regulation.
3. Which of the following enzymes is thiamine-dependent and essential for glucose oxidation in the brain?
A. Acetyl-CoA Carboxylase
B. Pyruvate Dehydrogenase Complex
C. Succinate Dehydrogenase
D. Succinyl-CoA Thiokinase
E. Transaldolase
The correct answer is B. Pyruvate Dehydrogenase Complex: The pyruvate dehydrogenase complex (PDC) catalyzes the conversion of pyruvate to acetyl-CoA, a critical step in glucose oxidation. It requires thiamine pyrophosphate (TPP) as a cofactor. In the brain, which relies heavily on glucose for energy, PDC plays a crucial role in maintaining energy metabolism. Thiamine deficiency impairs PDC function, leading to neurological disorders like Wernicke-Korsakoff syndrome.
Incorrect Options
A. Acetyl-CoA Carboxylase: This enzyme is involved in fatty acid synthesis, not glucose oxidation, and does not require thiamine.
C. Succinate Dehydrogenase: This enzyme participates in the TCA cycle and the electron transport chain but does not depend on thiamine.
D. Succinyl-CoA Thiokinase: While it catalyzes a step in the TCA cycle, it is not thiamine dependent.
E. Transaldolase: This enzyme functions in the pentose phosphate pathway, and its activity does not involve thiamine.
4. Which of the following components of the TCA cycle cannot be utilized for gluconeogenesis?
A. Acetyl-CoA
B. Alpha-Ketoglutarate
C. Malate
D. Oxaloacetate
E. Succinate
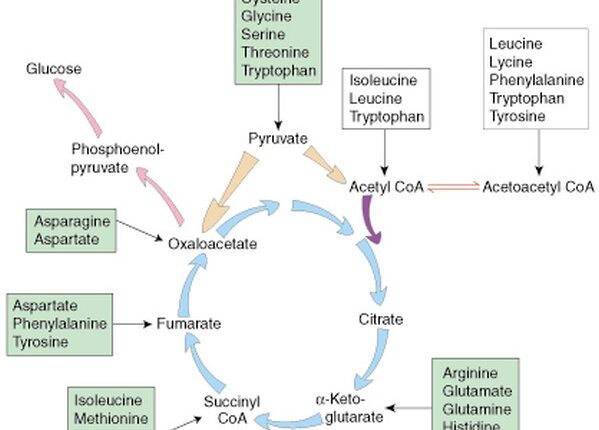
The correct answer is A. Acetyl-CoA: Acetyl-CoA cannot be converted into glucose via gluconeogenesis because the two carbons from acetyl-CoA enter the TCA cycle and are lost as CO₂ during the cycle. This prevents the net formation of glucose from acetyl-CoA, making it unusable for gluconeogenesis.
Incorrect Options
B. Alpha-Ketoglutarate: Alpha-ketoglutarate can be converted to oxaloacetate and used in gluconeogenesis.
C. Malate: Malate can be transported out of the mitochondria, converted to oxaloacetate, and participate in gluconeogenesis.
D. Oxaloacetate: Oxaloacetate is a direct precursor for phosphoenolpyruvate (PEP), a critical intermediate in gluconeogenesis.
E. Succinate: Succinate can be converted through the TCA cycle to malate and subsequently used for gluconeogenesis.
5. A 20-year-old female with a history of heavy menstruation and moderate to severe pyruvate dehydrogenase complex deficiency has been prescribed a ketogenic diet along with iron therapy. Which of the following TCA cycle intermediates would help her utilize ketone bodies and also promote heme synthesis?
A. Malate
B. Succinyl-CoA
C. Oxaloacetate
D. Fumarate
E. Succinate
The correct answer is B. Succinyl-CoA. Succinyl-CoA plays a dual role:
Ketone Body Utilization: It participates in the TCA cycle to help metabolize ketone bodies, providing energy, especially critical when carbohydrates are limited in a ketogenic diet.
Heme Synthesis: Succinyl-CoA combines with glycine to form δ-aminolevulinic acid (ALA), which is the first step in the heme biosynthesis pathway. Iron therapy will also complement this pathway by providing the necessary metal for heme production.
The incorrect options are:
A. Malate: Malate is a TCA cycle intermediate involved in the malate-aspartate shuttle, which helps transfer electrons from NADH across the mitochondrial membrane. It also plays a role in gluconeogenesis by converting into oxaloacetate. However, malate is not directly involved in ketone body utilization or heme synthesis.
C. Oxaloacetate: Oxaloacetate is crucial for gluconeogenesis and acts as a substrate in the TCA cycle by combining with acetyl-CoA to form citrate. While it plays a vital role in energy metabolism, it is not involved in ketone body metabolism or heme synthesis.
D. Fumarate: Fumarate is an intermediate in the TCA cycle, produced from succinate and converted into malate. Though it is essential in energy production, it does not contribute to ketone body metabolism or the biosynthesis of heme.
E. Succinate: Succinate participates in the TCA cycle by being converted into fumarate and plays a role in complex II of the electron transport chain. While it is essential for ATP generation, it is not directly involved in either ketone body metabolism or heme synthesis.
6. A 40-year-old man visits the emergency department due to severe abdominal pain, nausea, and vomiting. The patient is a chronic smoker, smoking half a pack of cigarettes daily. Blood tests reveal elevated lactate levels. Further evaluation suggests niacin (vitamin B3) deficiency, likely exacerbated by his poor diet and smoking. Decreased activity of which of the following enzymes best explains the patient’s condition?
A. Glucokinase
B. Pyruvate carboxylase
C. Pyruvate dehydrogenase
D. Pyruvate kinase
E. Succinate dehydrogenase
The correct answer is C. Pyruvate Dehydrogenase. Niacin deficiency leads to reduced NAD+ levels, impairing pyruvate dehydrogenase (PDH), which converts pyruvate to acetyl-CoA. When PDH activity is reduced, pyruvate accumulates and is converted into lactate, resulting in lactic acidosis. Chronic smoking further exacerbates oxidative stress and nutrient deficiencies, worsening the condition.
Incorrect Options: All other enzymes are not NAD+ dependent and, therefore, will not be affected by niacin deficiency;
7. A 4-year-old child with a history of liver cirrhosis presents to the emergency department with convulsions. The physician suspects that the convulsions are due to a deficiency of an inhibitory neurotransmitter, which plays a key role in preventing overexcitation of neurons. Which of the following TCA cycle intermediates serves as a precursor for the synthesis of this neurotransmitter?
A. Malate
B. Succinyl-CoA
C. Oxaloacetate
D. Fumarate
E. α-ketoglutarate
The correct answer is E. α-ketoglutarate. Glutamate is a critical precursor for the synthesis of γ-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the brain. In liver dysfunction, such as cirrhosis, disturbances in amino acid metabolism can deplete neurotransmitter precursors, leading to GABA deficiency and increased risk of seizures. Glutamate itself is derived from α-ketoglutarate, a TCA cycle intermediate, making it essential for normal neurotransmitter synthesis.
Incorrect Options:
A. Malate: An intermediate in the TCA cycle but not involved in neurotransmitter synthesis.
B. Succinyl-CoA: Plays a role in heme synthesis, not neurotransmitter production.
C. Oxaloacetate: Important in gluconeogenesis but not directly linked to GABA synthesis.
D. Fumarate: A TCA cycle intermediate with no role in neurotransmitter metabolism.
8. A 34-year-old homeless man reports to the emergency department due to numbness and “pins and needles” sensations in his legs. He also has painful lesions on his lips and the corners of his mouth. He drinks alcohol daily and has a history of intravenous heroin use. Laboratory evaluations show a very low level of riboflavin excretion in urine. The activity of which of the following enzymes might have been directly impaired in this patient?
A. Glycerladehyde-3-phosphate dehydrogenase
B. Isocitrate dehydrogenase
C. Malate dehydrogenase
D. Succinate dehydrogenase
E. Glutamate dehydrogenase
The correct answer is D. Succinate dehydrogenase: Riboflavin (vitamin B2) is essential for the synthesis of FAD (flavin adenine dinucleotide), a cofactor for several important metabolic enzymes, including succinate dehydrogenase. Succinate dehydrogenase plays a key role in both the TCA cycle and the electron transport chain, converting succinate to fumarate while transferring electrons to coenzyme Q. Riboflavin deficiency can impair succinate dehydrogenase activity, leading to metabolic disturbances that may contribute to the patient’s symptoms.
Incorrect Options:
A. Glyceraldehyde-3-phosphate dehydrogenase: This enzyme requires NAD+, not FAD, as a cofactor.
B. Isocitrate dehydrogenase: This enzyme depends on NAD+ or NADP+, not FAD.
C. Malate dehydrogenase: Uses NAD+ rather than FAD for catalysis.
E. Glutamate dehydrogenase: Requires NAD+ or NADP+, not FAD, for its activity.
9. A 2-month-old boy presents with irritability, vomiting, decreased urine output, and moderate respiratory distress. He is exclusively breastfed but hasn’t tolerated feeds since the previous day. Physical exam reveals hepatomegaly and chest radiography shows cardiomegaly. Laboratory tests indicate impaired carbohydrate metabolism, increased serum lactate levels, and decreased erythrocyte transketolase activity. Which of the following enzymes is most likely impaired in this patient?
A. Galactose-1-phosphate uridyl transferase
B. Glucokinase
C. Glucose-6-phosphatase
D. Lactate dehydrogenase
E. Pyruvate dehydrogenase
The correct answer is E. Pyruvate dehydrogenase: The key finding in this case is elevated serum lactate along with decreased erythrocyte transketolase activity. Decreased transketolase activity suggests a thiamine (vitamin B1) deficiency or dysfunction. Pyruvate dehydrogenase (PDH), which converts pyruvate to acetyl-CoA for entry into the TCA cycle, requires thiamine as a cofactor. When PDH is impaired, pyruvate accumulates and is shunted toward lactate production, leading to lactic acidosis, cardiomegaly, and hepatomegaly, as observed in this child.
Incorrect Options:
A. Galactose-1-phosphate uridyl transferase: Deficiency causes galactosemia, presenting with jaundice, hepatomegaly, and cataracts, but not elevated lactate or transketolase deficiency.
B. Glucokinase: A defect in glucokinase leads to issues with glucose sensing, contributing to diabetes, but it does not cause lactic acidosis or thiamine-related symptoms.
C. Glucose-6-phosphatase: Deficiency results in von Gierke disease, with hypoglycemia and hepatomegaly, but does not directly impair PDH or increase lactate levels.
D. Lactate dehydrogenase: Elevated lactate levels are the result of PDH deficiency, not the cause. LDH activity would increase to convert excess pyruvate to lactate.
10. A 25-year-old man consumes a high-carbohydrate meal after an intense workout. To efficiently metabolize the incoming glucose, the body must activate the pyruvate dehydrogenase (PDH) complex. Which of the following ratios is expected to be elevated to inhibit PDH kinase, thereby activating PDH complex?
A. [Acetyl-CoA]/[CoASH]
B. [ATP]/[ADP]
C. [ATP]/[AMP]
D. [Insulin]/[Glucagon]
E. [NADH]/[NAD+]
The correct answer is D. [Insulin]/[Glucagon. After a high-carbohydrate meal, insulin levels rise, and the insulin/glucagon ratio increases. Insulin promotes the dephosphorylation and activation of PDH by inhibiting PDH kinase, the enzyme that normally phosphorylates and inactivates PDH. This ensures that glucose-derived pyruvate is efficiently converted to acetyl-CoA, promoting its oxidation in the TCA cycle for energy production.
Incorrect Options:
A. [Acetyl-CoA]/[CoASH]:
An elevated acetyl-CoA/CoASH ratio signals sufficient energy, leading to inhibition of PDH to shift metabolism toward fat storage.
B. [ATP]/[ADP]:
A high ATP/ADP ratio indicates energy sufficiency and would inhibit PDH, not activate it.
C. [ATP]/[AMP]:
Similar to the ATP/ADP ratio, a high ATP/AMP ratio indicates high energy levels and leads to the inhibition of PDH.
E. [NADH]/[NAD+]:
An elevated NADH/NAD+ ratio suggests that oxidative metabolism is slowed, signaling a reduced need for PDH activation.
