Library
Starvation induced metabolic alterations
- March 16, 2020
- Posted by: Namrata Chhabra
- Category: Case based discussions Case based multiple choice questions Metabolism of Carbohydrates Multiple-choice questions USMLE Content USMLE Style questions USMLE styled question bank
A 23 –year- old female was brought for consultation by her mother, who was troubled by her daughter’s continuous fatigue, dizziness, and loss of weight. The patient was 6 feet 2 inches tall and weighed 100 pounds. Further questioning revealed that the young woman had been virtually fasting for four months, hoping to obtain a ‘skinny figure’ as a prelude to a career in modeling. Physical examination revealed dehydration and a fruity odor in her breath.
Laboratory results revealed – Blood glucose 50 mg%.
Which substance would most likely be detected in abnormally high concentration upon the patient’s urine test?
A) Protein
B) Hemoglobin
C) Acetoacetate
D) Lactate
E) Pyruvate
The correct answer is- Acetoacetate.
The patient shows many signs of Anorexia Nervosa (AN), which is an eating disorder. The etiology of AN is unknown but appears to involve a combination of psychological, biological, and cultural risk factors. The condition is characterized by aversion to food that leads to a state of fasting and emaciation. Patients often have a distorted image of their body weight or shape and are unconcerned by the serious health consequences of their low weight. As weight loss progresses, the fear of gaining weight grows; dieting becomes stricter; and psychological, behavioral, and medical aberrations increase.
Metabolic alterations
Blood glucose homeostasis
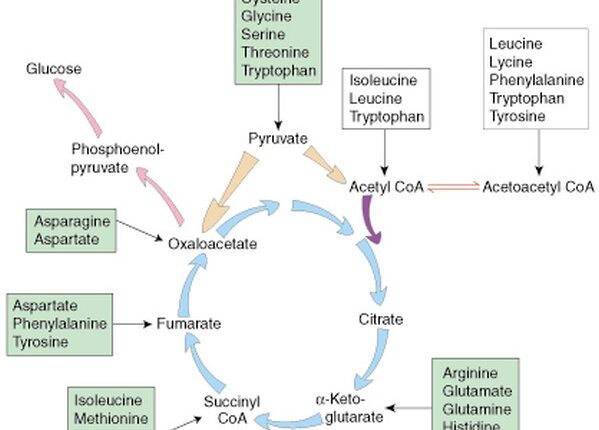
Liver glycogen is exhausted on the first day of fasting. After several months of near starvation, the blood glucose in these patients is maintained by gluconeogenesis, primarily from amino acids mobilized from tissue proteins (figure-1). The impaired conversion of amino acids to glucose is responsible for producing hypoglycemia in these patients.
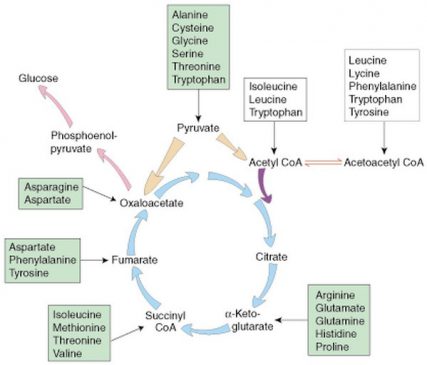
Figure-1- All the intermediates of the TCA cycle, beyond α- Ketoglutarate are glucogenic since they ultimately produce oxaloacetate that is channeled towards the pathway of gluconeogenesis. Acetyl co A is not glucogenic, as firstly, the conversion of pyruvate to Acetyl Co-A is irreversible and secondly, in the TCA cycle, both of its carbons are lost in the form of CO2, hence it has nothing to contribute towards Glucose production.
Implications of hypoglycemia
Gluconeogenesis depletes the supply of oxaloacetate, which is essential for the entry of acetyl CoA into the citric acid cycle (figure-1). Consequently, the liver produces large quantities of ketone bodies, which are released into the blood (figure-2). After several weeks of starvation, ketone bodies become the major fuel of the brain. A person’s survival time is mainly determined by the size of the triacylglycerol depot.
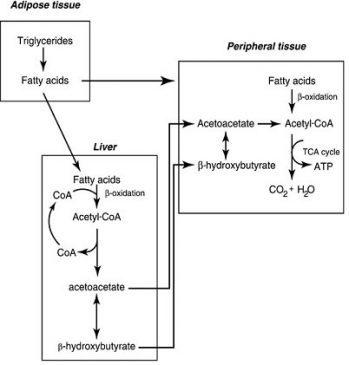
Figure-2- During starvation, hypoglycemia causes the release of glucagon that promotes lipolysis in the adipose tissue. The fatty acids released are transported to the liver. They are oxidized to provide energy to the liver cells. The end product, Acetyl Co A, cannot be completely utilized in the TCA cycle, as it is in a state of suppression due to mobilization of oxaloacetate towards the pathway of gluconeogenesis. Acetyl Co-A is diverted to the pathway of ketogenesis. The ketone bodies are transported through the blood to the peripheral cells, where they are used as fuel molecules to provide energy. The ketone bodies are produced in the liver but they are utilized in the peripheral cells. The enzyme (thiophorase) for their utilization is present in all the peripheral cells except the liver. In contrast, the enzymes for ketogenesis (HMG Co-A synthase and HMG Co-A lyase) are present only in the liver mitochondria).
As a result of ketosis, the blood pH becomes acidic, since the ketone bodies are themselves acidic (ionic at pH 7.4), and are excreted in the form of neutral salts. Hence they deplete the alkali reserve of the body, causing acidosis.
Excess ketone bodies are excreted in the urine, causing ketonuria. Acetoacetate is the primary ketone body. The other two ketone bodies, beta-hydroxybutyrate and acetone, are derived from acetoacetate. Beta-hydroxybutyrate is the major ketone body in urine; acetone is excreted through the breath. Acetone like smell is observed in patients of ketoacidosis, and it is a diagnostic sign of ketoacidosis.
In the given options, acetoacetate is the correct option considering the clinical state of hypoglycemia induced ketoacidosis.
As regards other options
A) Protein
B) Hemoglobin
C) Acetoacetate
D) Lactate
E) Pyruvate
Protein cannot be there in urine in this condition, as the kidney functions are normal. Similarly, hemoglobin also cannot be found, since there is no apparent cause of hemoglobinuria. Lactic acidosis is not there; hence lactate cannot be excreted in the urine. Pyruvate is not found in urine; it is mostly utilized in many pathways.
Hence Acetoacetate is the most appropriate option.
Author:Namrata Chhabra
Leave a Reply Cancel reply
You must be logged in to post a comment.
