Library
Oncogenes in Human Cancer: A Deep Dive
- February 27, 2025
- Posted by: Namrata Chhabra
- Category: USMLE Content Cancer Cancer Lecture notes Quick revisions
Oncogenes in Human Cancer: A Deep Dive
Cancer is one of the leading causes of mortality worldwide, and oncogenes play a pivotal role in its development. Oncogenes are cancer susceptibility genes that arise from normal genes, called proto-oncogenes, which are essential for cell growth and differentiation. However, under specific conditions, proto-oncogenes can transform into oncogenes, leading to uncontrolled cell proliferation and tumor formation.
What Are Proto-Oncogenes?
Proto-oncogenes are crucial for normal cellular processes. They regulate cell growth, differentiation, and apoptosis by participating in signaling pathways mediated by growth factors, membrane receptors, and intracellular signaling molecules like kinases and G proteins. When functioning correctly, these pathways ensure orderly cell proliferation. However, disruptions may lead to tumorigenesis.
How Do Proto-Oncogenes Become Oncogenes?
Proto-oncogenes can transform into oncogenes due to exposure to various carcinogens such as chemicals, radiation, or viruses, as well as due to genetic predisposition. This transformation leads to either overproduction of gene products or creation of abnormal gene products, ultimately resulting in malignant transformation of normal cells into cancerous cells.
Key Mechanisms of Oncogene Activation
There are four primary mechanisms through which oncogenes become activated:
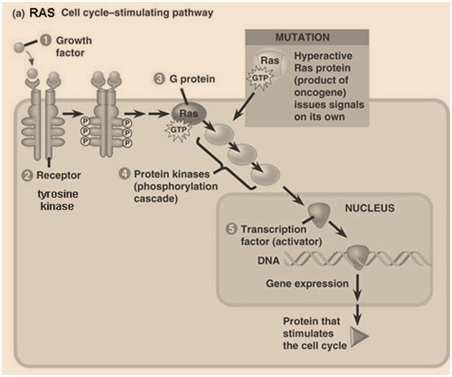
- Point Mutation
Point mutations in specific genes are a common mechanism of oncogene activation. For example, mutations in the RAS gene family (HRAS, KRAS, NRAS) are found in up to 85% of pancreatic cancers and 50% of colon cancers. Mutations in codons 12, 13, or 61 result in the continuous activation of Ras protein, leading to chronic stimulation of adenylate cyclase and excessive cellular proliferation (Figure 1).

Figure 1- showing the effects of activated RAS protein. Growth factor- Receptor binding stimulates tyrosine kinase activity that stimulates the Ras protein, a G protein that is active when bound to GTP. Active Ras protein activates adenylate cyclase and a phosphorylation cascade is triggered. Mutated Ras protein remains active due to inability to replace GTP by GDP, resulting in phosphorylation of cellular proteins, and more synthesis of cell cycle regulatory proteins, and thereby malignant transformation of the cell.
Mechanism of Ras Activation
The gene product (p21) is related to the G protein that modulates the activity of adenylate cyclase, playing a key role in cellular responses to hormones and drugs. p21 also has GTPase activity, which helps terminate hormonal action. However, mutations in p21 alter its conformation and reduce its GTPase activity. This diminished activity results in chronic stimulation of adenylate cyclase, increasing cAMP levels and leading to uncontrolled cell growth and malignant transformation.
- Gene Amplification
Gene amplification leads to excessive production of oncogenic gene products. For example, in methotrexate-resistant tumors, the dihydrofolate reductase gene is amplified, increasing enzyme activity up to 400-fold. Similarly, oncogenes may undergo amplification, accelerating tumor progression and malignancy (Figure 2).

Figure 2 shows the mechanism of gene amplification
- Chromosomal Rearrangement
Chromosomal alterations provide crucial insights into genetic changes in cancer. While solid tumors show complex chromosomal variations, myeloid and lymphoid malignancies often involve simple translocations.
Examples:
- Burkitt’s Lymphoma: A reciprocal translocation between chromosomes 8 and 14 places the C-MYC gene under the control of immunoglobulin enhancers, leading to excessive transcription and tumor growth (Figure 3).

Figure 3 shows the chromosomal translocation in Burkitt’s lymphoma
- Philadelphia Chromosome in Chronic Myelogenous Leukemia (CML):
A translocation between chromosome 9 (ABL oncogene) and chromosome 22 (BCR region) creates the BCR-ABL fusion gene (Figure 4), which activates signal transduction pathways that promote uncontrolled cell growth. The targeted therapy Imatinib effectively blocks BCR-ABL activity and has revolutionized CML treatment.

Figure 4 shows the Philadelphia chromosome in chronic myelogenous leukemia. Chromosomes 9 and 22 are involved in this translocation, forming the BCR-ABL fusion gene.
- Insertional Mutagenesis
Certain viruses can cause cancer through insertional mutagenesis by integrating viral DNA into the host genome.
- Promoter Insertion: The long terminal repeat (LTR) sequences of retroviruses function as promoters, enhancing transcription of proto-oncogenes like C-MYC, resulting in tumorigenesis (Figure 5).
- Enhancer Insertion: Viral enhancers activate gene expression even when inserted downstream or in reverse orientation, causing increased transcription and uncontrolled cell growth.

Figure-5- Proto-oncogene activation by insertional mutagenesis of MMTV-(a) Insertion of viral genomic DNA into somatic cellular DNA in close proximity of a silent oncogene. (b) Inserted proviral DNA induces the transcription of the oncogene.
Consequences of Oncogene Activation
Oncogene overexpression results in increased gene products that drive malignant transformation. In some cases, mutations in regulatory genes cause structurally abnormal key regulatory proteins, accelerating cancer progression.
However, oncogene activation alone is insufficient for cancer development. A combination of oncogene activation and tumor suppressor gene inactivation is typically required for full malignant transformation. Tumor suppressor genes like TP53 and RB1 act as cell cycle regulators. When inactivated, unchecked cell proliferation leads to cancer.
Functions of Oncogene Products
The protein products of oncogenes play a central role in cancer progression by:
- Activating intracellular pathways that control growth.
- Regulating the cell cycle via DNA-binding proteins.
- Mimicking growth factors or acting as activated growth factor receptors, driving excessive cellular proliferation.
Conclusion
Oncogene activation is a fundamental event in cancer progression, triggered by diverse mechanisms such as point mutations, gene amplification, chromosomal translocations, and viral insertional mutagenesis. These genetic alterations drive uncontrolled cell growth, often compounded by the inactivation of tumor suppressor genes.
Understanding oncogene mechanisms has led to groundbreaking targeted therapies like Imatinib for CML, offering more effective and personalized cancer treatments. Future research into oncogene-targeted therapies holds promise for innovative breakthroughs in cancer care.
